Introduction to insulin resistance
Insulin resistance is a condition that affects millions of people worldwide, yet many are unaware of its existence or the potential impact it can have on their health. As a writer with a keen interest in health and wellness, I aim to shed light on this critical topic, providing a comprehensive understanding of what insulin resistance entails and how it can influence various aspects of our well-being.
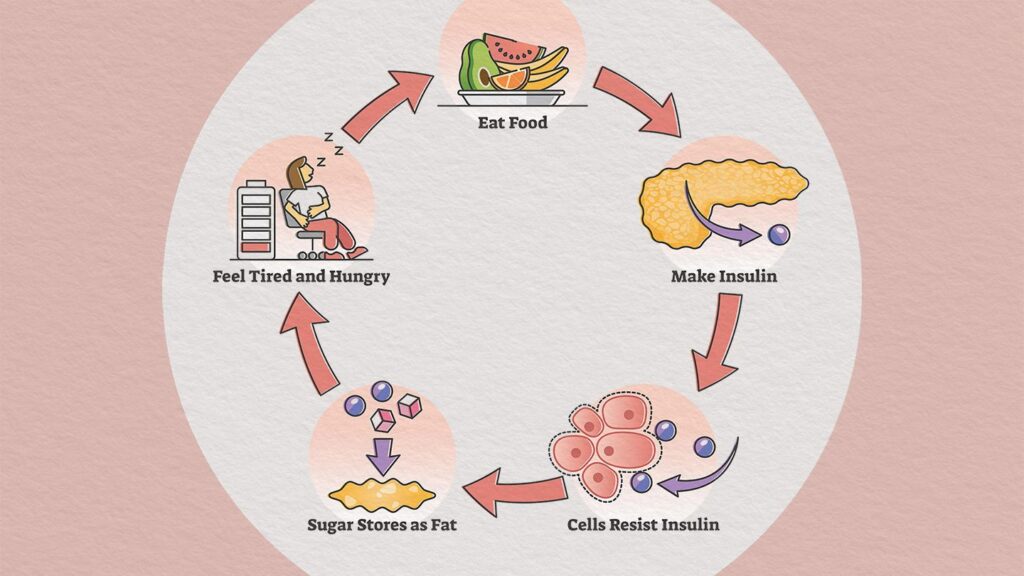
Insulin is a hormone produced by the pancreas, responsible for regulating blood sugar levels by facilitating the absorption of glucose into cells for energy production or storage. When the body becomes resistant to insulin, it fails to effectively utilize the insulin produced, leading to an accumulation of glucose in the bloodstream. This condition is known as insulin resistance, and it can have far-reaching consequences if left unaddressed.
In this article, we will delve into the intricacies of insulin resistance, exploring its causes, symptoms, diagnosis, complications, and treatment options. Additionally, we will discuss lifestyle changes that can help manage and potentially prevent this condition, empowering you to take proactive steps towards better health.
How insulin resistance affects your health
Insulin resistance can have a profound impact on various aspects of your health, extending beyond just blood sugar regulation. When the body becomes resistant to insulin, it can trigger a cascade of effects that affect multiple organ systems and increase the risk of developing several chronic conditions.
- Impaired glucose metabolism: As insulin resistance progresses, the body struggles to effectively utilize glucose, leading to elevated blood sugar levels (hyperglycemia). Chronic hyperglycemia can damage blood vessels, nerves, and organs, increasing the risk of complications like neuropathy, retinopathy, and kidney disease.
- Increased risk of type 2 diabetes: Insulin resistance is a precursor to type 2 diabetes, a condition characterized by the body’s inability to produce or effectively utilize insulin. If left unmanaged, insulin resistance can progress to type 2 diabetes, which carries its own set of potential complications.
- Cardiovascular implications: Insulin resistance is closely linked to an increased risk of developing cardiovascular diseases, such as hypertension, atherosclerosis, and stroke. It can contribute to the development of dyslipidemia (abnormal cholesterol and triglyceride levels), inflammation, and endothelial dysfunction, all of which are risk factors for heart disease.
- Metabolic syndrome: Insulin resistance is a key component of metabolic syndrome, a cluster of conditions that includes abdominal obesity, high blood pressure, high triglycerides, low HDL (good) cholesterol levels, and elevated blood sugar. Metabolic syndrome significantly increases the risk of developing type 2 diabetes, heart disease, and stroke.
- Polycystic ovary syndrome (PCOS): Insulin resistance is closely associated with PCOS, a hormonal disorder that can cause irregular menstrual cycles, infertility, and an increased risk of developing other health issues like type 2 diabetes and cardiovascular disease.
By understanding the far-reaching effects of insulin resistance, we can appreciate the importance of early detection and management to mitigate the potential risks and complications associated with this condition.
Causes of insulin resistance
Insulin resistance can arise from various factors, including genetic predisposition, lifestyle choices, and underlying medical conditions. It is essential to understand these causes to develop effective strategies for prevention and management.
- Genetics: Certain genetic variations can increase an individual’s susceptibility to developing insulin resistance. While genetics alone may not be the sole cause, it can contribute to the development of this condition, particularly when combined with other risk factors.
- Obesity and overweight: Excess body weight, especially abdominal obesity, is strongly linked to insulin resistance. Adipose tissue (fat cells) can release inflammatory substances and hormones that interfere with insulin signaling, contributing to insulin resistance.
- Sedentary lifestyle: Physical inactivity and a lack of regular exercise can increase the risk of insulin resistance. Exercise helps to enhance insulin sensitivity and glucose uptake by muscles, promoting better blood sugar regulation.
- Poor diet: A diet high in refined carbohydrates, saturated fats, and processed foods can contribute to insulin resistance. These foods can lead to inflammation, oxidative stress, and an imbalance in hormones and metabolic processes, all of which can impair insulin sensitivity.
- Aging: As we age, the risk of developing insulin resistance tends to increase. This is due to various factors, such as changes in body composition, decreased physical activity, and alterations in hormonal levels.
- Certain medical conditions: Conditions like polycystic ovary syndrome (PCOS), non-alcoholic fatty liver disease (NAFLD), and certain hormonal disorders can increase the risk of developing insulin resistance.
- Stress and sleep disturbances: Chronic stress and poor sleep quality can disrupt hormonal balances and contribute to the development of insulin resistance.
By understanding the various causes of insulin resistance, we can identify potential risk factors and take proactive steps to mitigate their impact through lifestyle modifications and medical interventions, if necessary.
Symptoms of insulin resistance
In the early stages, insulin resistance may not present any noticeable symptoms, making it challenging to detect without proper screening. However, as the condition progresses, certain signs and symptoms may become apparent. It is crucial to be aware of these potential indicators to seek timely medical evaluation and intervention.
- Increased thirst and frequent urination: As the body struggles to regulate blood sugar levels, excess glucose can spill into the urine, leading to increased thirst and frequent urination.
- Fatigue and lethargy: Insulin resistance can interfere with the body’s ability to effectively utilize glucose for energy production, resulting in feelings of fatigue and lethargy.
- Unexplained weight gain or difficulty losing weight: Insulin resistance can contribute to weight gain, particularly around the abdominal area, and make weight loss efforts more challenging.
- Skin changes: Some individuals with insulin resistance may experience darkening of the skin in certain areas, such as the armpits, neck, and groin, a condition known as acanthosis nigricans.
- Irregular menstrual cycles and infertility: Women with insulin resistance may experience irregular menstrual cycles, polycystic ovary syndrome (PCOS), and fertility issues due to hormonal imbalances.
- Increased hunger and cravings: Insulin resistance can disrupt the body’s ability to regulate appetite hormones, leading to increased hunger and cravings, particularly for sugary and carbohydrate-rich foods.
It is important to note that these symptoms can also be associated with other medical conditions, and their presence does not necessarily confirm insulin resistance. If you experience any of these symptoms, it is advisable to consult a healthcare professional for proper evaluation and diagnosis.
Diagnosing insulin resistance
Diagnosing insulin resistance typically involves a combination of physical examinations, medical history evaluation, and laboratory tests. Healthcare professionals may employ the following methods to assess insulin resistance:
- Physical examination: Your healthcare provider will conduct a thorough physical examination, including measurements of body weight, height, waist circumference, and blood pressure. These assessments can provide insights into potential risk factors for insulin resistance, such as obesity or hypertension.
- Medical history: Your healthcare provider will review your medical history, including any pre-existing conditions, family history, and lifestyle factors that may contribute to insulin resistance.
- Blood tests: Several blood tests can help evaluate insulin resistance and related conditions:
- Fasting blood glucose test: This test measures your blood sugar levels after an overnight fast, providing insights into your body’s ability to regulate glucose.
- Oral glucose tolerance test (OGTT): This test involves measuring blood sugar levels before and after consuming a sugary drink, assessing how effectively your body processes and responds to glucose.
- Hemoglobin A1C (HbA1c) test: This test provides an average measure of your blood sugar levels over the past 2-3 months, helping to identify patterns of elevated blood sugar.
- Insulin levels: Your healthcare provider may order tests to measure your fasting insulin levels or conduct an insulin resistance test, such as the homeostatic model assessment of insulin resistance (HOMA-IR).
- Additional tests: Depending on your individual circumstances, your healthcare provider may recommend additional tests to assess related conditions or complications, such as lipid profiles (cholesterol and triglyceride levels), liver function tests, or imaging studies.
It is important to note that the diagnosis of insulin resistance is often based on a combination of factors, including clinical findings, laboratory results, and risk factors. Your healthcare provider will interpret these results in the context of your overall health and medical history to determine the appropriate course of action.
Complications of insulin resistance
If left unmanaged, insulin resistance can lead to various complications that can significantly impact your overall health and well-being. It is crucial to be aware of these potential complications to understand the importance of early detection and effective management strategies.
- Type 2 diabetes: Insulin resistance is a major risk factor for developing type 2 diabetes, a chronic condition characterized by elevated blood sugar levels due to the body’s inability to produce or effectively utilize insulin. Uncontrolled diabetes can lead to serious complications, including nerve damage, kidney disease, vision problems, and an increased risk of cardiovascular diseases.
- Cardiovascular diseases: Insulin resistance is closely linked to an increased risk of developing cardiovascular diseases, such as hypertension, atherosclerosis (buildup of plaque in the arteries), and an increased risk of heart attacks and strokes. This is due to the adverse effects of insulin resistance on lipid levels, inflammation, and endothelial function (the inner lining of blood vessels).
- Metabolic syndrome: Insulin resistance is a key component of metabolic syndrome, a cluster of conditions that includes abdominal obesity, high blood pressure, high triglycerides, low HDL (good) cholesterol levels, and elevated blood sugar. Metabolic syndrome significantly increases the risk of developing type 2 diabetes, heart disease, and stroke.
- Polycystic ovary syndrome (PCOS): Insulin resistance is closely associated with PCOS, a hormonal disorder that can cause irregular menstrual cycles, infertility, and an increased risk of developing other health issues like type 2 diabetes and cardiovascular disease.
- Non-alcoholic fatty liver disease (NAFLD): Insulin resistance can contribute to the accumulation of fat in the liver, leading to non-alcoholic fatty liver disease (NAFLD). NAFLD can progress to more severe conditions like non-alcoholic steatohepatitis (NASH) and potentially increase the risk of liver cirrhosis and liver failure.
- Sleep apnea: Insulin resistance has been linked to an increased risk of developing sleep apnea, a condition characterized by interrupted breathing during sleep, which can further exacerbate insulin resistance and other health issues.
- Cancer risk: Emerging research suggests a potential link between insulin resistance and an increased risk of certain types of cancer, such as breast, colon, and endometrial cancers, although the mechanisms are not fully understood.
By recognizing the potential complications associated with insulin resistance, individuals can take proactive steps to manage their condition and reduce the risk of developing these serious health issues.
Treatment options for insulin resistance
Treating insulin resistance typically involves a multifaceted approach that combines lifestyle modifications, medications, and, in some cases, surgical interventions. The specific treatment plan will depend on the severity of the condition, the presence of any underlying medical conditions, and individual factors.
- Lifestyle modifications:
- Diet: Adopting a healthy, balanced diet low in refined carbohydrates, processed foods, and saturated fats can help improve insulin sensitivity. Incorporating more whole foods, fiber-rich vegetables, lean proteins, and healthy fats is recommended.
- Exercise: Regular physical activity, such as aerobic exercise and strength training, can enhance insulin sensitivity by improving glucose uptake by muscles and reducing body fat.
- Weight management: Achieving and maintaining a healthy body weight through a combination of diet and exercise can significantly improve insulin sensitivity and reduce the risk of complications associated with insulin resistance.
- Medications:
- Metformin: This is a commonly prescribed medication for individuals with insulin resistance or type 2 diabetes. It helps to improve insulin sensitivity and reduce glucose production by the liver.
- Thiazolidinediones (TZDs): These medications, such as pioglitazone and rosiglitazone, can improve insulin sensitivity by targeting specific receptors involved in glucose and lipid metabolism.
- Glucagon-like peptide-1 (GLP-1) agonists: These injectable medications, like liraglutide and semaglutide, can improve insulin sensitivity and promote weight loss, making them beneficial for individuals with insulin resistance.
- Insulin therapy: In some cases, particularly for individuals with advanced insulin resistance or type 2 diabetes, insulin injections may be necessary to help manage blood sugar levels.
- Surgical interventions:
- Bariatric surgery: For individuals with severe obesity and insulin resistance, bariatric surgery (such as gastric bypass or sleeve gastrectomy) may be recommended. These procedures can lead to significant weight loss and improve insulin sensitivity.
It is essential to work closely with a healthcare professional to develop a personalized treatment plan that addresses your specific needs and circumstances. Regular monitoring and adjustments may be necessary to achieve optimal management of insulin resistance and prevent or delay the progression of related complications.
Lifestyle changes to manage insulin resistance
While medical interventions play a crucial role in managing insulin resistance, adopting a healthy lifestyle is equally important. By making sustainable changes to your daily habits, you can significantly improve insulin sensitivity, reduce the risk of complications, and potentially reverse the progression of insulin resistance.
- Adopt a balanced and nutrient-dense diet:
- Focus on whole, unprocessed foods like vegetables, fruits, lean proteins, whole grains, and healthy fats.
- Limit your intake of refined carbohydrates, added sugars, and saturated fats, as they can contribute to insulin resistance.
- Increase your fiber intake from sources like fruits, vegetables, legumes, and whole grains, as fiber can help regulate blood sugar levels.
- Stay hydrated by drinking plenty of water and unsweetened beverages.
- Incorporate regular physical activity:
- Aim for at least 150 minutes of moderate-intensity aerobic exercise or 75 minutes of vigorous-intensity exercise per week.
- Include strength training exercises at least two days per week to build and maintain muscle mass, which can improve insulin sensitivity.
- Incorporate activities that you enjoy, such as walking, cycling, swimming, or dancing, to increase adherence.
- Break up prolonged periods of inactivity by taking regular breaks and engaging in light physical activity throughout the day.
- Achieve and maintain a healthy body weight:
- Work towards achieving and maintaining a healthy body mass index (BMI) through a combination of a balanced diet and regular physical activity.
- Focus on gradual and sustainable weight loss, if necessary, as rapid weight loss can sometimes worsen insulin resistance initially.
- Manage stress and prioritize sleep:
- Engage in stress-reducing activities like meditation, yoga, deep breathing exercises, or other relaxation techniques.
- Aim for 7-9 hours of quality sleep per night, as sleep deprivation and poor sleep quality can contribute to insulin resistance.
- Quit smoking and limit alcohol consumption:
- Smoking and excessive alcohol intake can exacerbate insulin resistance and increase the risk of related complications.
- If you smoke, seek support to quit, and if you consume alcohol, limit your intake to moderate levels.
By incorporating these lifestyle changes into your daily routine, you can significantly improve your insulin sensitivity, reduce the risk of developing complications associated with insulin resistance, and potentially reverse the progression of the condition.
Prevention of insulin resistance
While certain risk factors for insulin resistance, such as genetics and aging, are beyond our control, there are proactive steps you can take to reduce your chances of developing this condition or delaying its onset.
- Maintain a healthy body weight: Achieving and maintaining a healthy body weight through a balanced diet and regular physical activity is one of the most effective ways to prevent insulin resistance. Excess body weight, particularly abdominal obesity, is a significant risk factor for insulin resistance.
- Engage in regular physical activity: Regular exercise, both aerobic and strength training, can improve insulin sensitivity and glucose metabolism. Aim for at least 150 minutes of moderate-intensity aerobic activity or 75 minutes of vigorous-intensity activity per week, combined with strength training exercises at least two days per week.
- Follow a nutrient-dense diet: Adopt a diet rich in whole, unprocessed foods like fruits, vegetables, lean proteins, whole grains, and healthy fats. Limit your intake of refined carbohydrates, added sugars, and saturated fats, as these can contribute to insulin resistance.
- Manage stress and prioritize sleep: Chronic stress and poor sleep quality can disrupt hormonal balances and contribute to the development of insulin resistance. Engage in stress-reducing activities and aim for 7-9 hours of quality sleep per night.
- Quit smoking and limit alcohol consumption: Smoking and excessive alcohol intake can increase the risk of insulin resistance and related complications. If you smoke, seek support to quit, and if you consume alcohol, limit your intake to moderate levels.
- Regular health check-ups: Schedule regular check-ups with your healthcare provider to monitor your risk factors, such as body weight, blood pressure, and blood sugar levels. Early detection and intervention can help prevent or delay the onset of insulin resistance.
By adopting a proactive and preventive approach, you can significantly reduce your risk of developing insulin resistance and its associated complications. It is crucial to recognize that small, sustainable lifestyle changes can have a profound impact on your overall health and well-being.
Conclusion
Insulin resistance is a complex and multifaceted condition that can have far-reaching consequences if left unaddressed. By understanding the causes, symptoms, and potential complications of insulin resistance, we can take proactive steps to manage and potentially prevent this condition.
Adopting a healthy lifestyle, which includes a balanced diet, regular physical activity, weight management, stress reduction, and adequate sleep, is crucial in improving insulin sensitivity and reducing the risk of developing related complications. Additionally, seeking medical advice and adhering to prescribed treatment plans can help effectively manage insulin resistance and prevent its progression.
Remember, insulin resistance is a condition that can be influenced by our daily choices and habits. By making informed decisions and taking proactive measures, we can take control of our health and reduce the burden of this condition on our overall well-being.If you suspect you may be experiencing symptoms of insulin resistance or have concerns about your risk factors, I encourage you to consult with a healthcare professional. Early detection and intervention can make a significant difference in managing this condition and preventing potential complications. Take charge of your health today by prioritizing a balanced lifestyle and seeking professional guidance when needed.